
How Bright Light Therapy Helps with Low Mood, Sleep Problems and Jet Lag
Last Revised November 2019

How Bright Light Therapy Helps with Low Mood, Sleep Problems and Jet Lag
By Daniel F. Kripke, M.D.
Last Revised November 2019
Using Antidepressant Drugs and Counseling
Remember the caution with which we started discussing light treatment of depression. You should check with your doctor. If you have significant depression, especially if you might have a major depressive disorder, if bad mood is keeping you from your normal activities, or you have any thought of hurting yourself, you should certainly get your doctor’s help. It is nice that self-managed light is sometimes sufficient for the mild problems, but please do not count on bright light alone if your depression is causing serious trouble.
This caution is similar to the caution with other health aids. An average person knows how to get some exercise, but if you have had a heart attack, you would need to discuss exercise with your doctor. An average person knows it is good to skip dessert, but if you have diabetes or a stomach ulcer, you need to discuss a detailed diet with your doctor. Similarly, people might try light for minor problems by themselves, but for serious depression, a doctor’s advice should always be sought.
We used to think about bright light as an alternative to the better-known treatments for depression, especially as an alternative to antidepressant medicines and counseling. That is not my viewpoint anymore. Experience shows that even when light treatment helps, it is often not enough. We realize now that light treatment works very well in combination with the antidepressant drugs. These are drugs like citalopram, amitriptyline, trazadone, and lithium – there are quite a few kinds which are good. In fact, it seems that bright light often works best along with antidepressant drugs. The benefits may multiply each other.
Requiring years of effort, a very carefully-designed randomizing controlled trial was done at psychiatric centers in Canada, comparing light treatment with placebo, with fluoxetine (one of the most popular antidepressants, e.g., Prozac brand), and with the combination of light treatment and fluoxetine.[29] The patients suffered nonseasonal major depressions. The outcome is summarized in the figure below: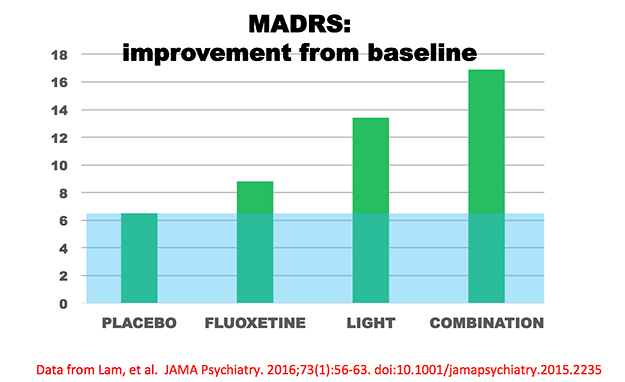
The MADRS is a quantitative estimate of the intensity of a patient’s depression. The figure above shows the amount that patients’ MADRS scores improved (depression scores decreased) from baseline to the end of eight weeks of treatment. The group that received only inactive placeboes improved 6.5 points, a typical combination of “placebo effect” and spontaneous remission in such trials. The blue shading shows this “placebo effect,” and the green bars extending above the blue show the amount the treated groups improved more than those with inactive treatment. The fluoxetine drug group improved 2.3 points more than the placebo group, a typical benefit size in controlled trials of fluoxetine. The light-treated group improved 6.9 points more than placebo, and the group receiving the combination of fluoxetine and light improved 10.4 points more. Note that the combined group experienced somewhat more benefit than the sum of improvements in the fluoxetine-alone and light-alone groups. To summarize this important study, not only was light treatment better than the no-treatment control, light also worked faster than fluoxetine and appeared to help more. Moreover, the combination of light treatment and fluoxetine was better than fluoxetine alone. Although the statistical analysis was not adequate to prove interaction, the combination of light treatment and fluoxetine appeared somewhat better than simple addition of the light-alone benefit plus the fluoxetine-alone benefit; that is, the two treatments appeared possibly synergistic and seemed to help each other. This study as well as other studies of combined treatment argue strongly for combining light treatment with antidepressant drugs.
There are some controlled trials assessing psychotherapeutic treatments versus light treatments versus their combination for SAD, showing possibly somewhat faster responses with light,[30] possibly more lasting freedom from relapse with CBT psychotherapy of depression,[31] but the best results with the combination. I think it appears likely that a combination of light and antidepressant drugs and CBT psychotherapy would be optimal.
I was formerly quite enthusiastic about the antidepressant medicines for outpatients. These medicines help millions of people. However, usage has grown so great that it is no longer clear that antidepressants are needed by everybody who is getting them. Moreover, recent critiques which examined the controlled drug trials that were not published (as well as the more favorable trials which the manufacturers published) have indicated that our appreciation of the antidepressant drugs may have become over-enthusiastic.[32] Realistically, for patients not depressed enough to be hospitalized, the amount of the benefit of the antidepressant drugs is usually very small. Nevertheless, depressed people in most cases do better with antidepressant medicines than without them. There have been literally hundreds of studies which prove that the antidepressant medicines provide more benefit than they do harm.[33]
Do not be scared by all the sensationalism about side effects which has appeared in certain news media. It is true that all antidepressant drugs have side effects, but so do water, sugar, salt, apples, oranges, and just about anything else in life. Compared to driving an automobile, much less a riding a bicycle or trying roller blades, antidepressant drugs are very safe. For most people who are really depressed, the side effects of antidepressant drugs are worth it. Talk to your doctor about it.
Counseling is also good for depression. There are new kinds of psychotherapy of depression that really do work. There have now been many studies which prove the benefits of modern psychotherapies of depression. A long time ago, I was trained in the old Freudian methods of treating depression (dream analysis and talk about childhood, for example), and I have to say that I do not believe that those old methods helped depression much. Doctors trained in the newer methods accomplish more. Psychotherapy certainly seems generally safe. In all probability, psychotherapy plus antidepressant drugs works better than the medicines used alone. There have been few good tests of the combinations of bright light and psychotherapy and no tests of combining bright light, medication and psychotherapy that I know of. There is every reason to think that these combinations would be safe and more effective than a single treatment. Indeed, the combination of bright light, antidepressant drugs, and psychotherapy might be the best for many people. I wish there were more results of clinical trials of light benefits to describe, but no treatment in medicine has been tested long-term in every possible combination with other treatments. Talk to your doctor about psychotherapy.
Bright light treatment for winter depression has been supported by dozens of studies demonstrating beneficial results (though there have been a few studies with unsuccessful results).[34] The Clinical Practice Guidelines issued by the U.S. Department of Health and Human Services[35] recognized bright light as a generally accepted treatment for winter depression.
Until recently, there were rather few studies of bright light treatment of nonseasonal depression; however, there are now dozens of controlled studies showing that bright light reduces symptoms in nonseasonal depression. The study of Lam et al. described above was the most conclusive study, but we might review some of the earlier ones.
Scientists rate how depressed patients are both before and after treatment using descriptive methods called depression rating scales. For example, a doctor who talked to the patient gives scores for how much the patient seemed sad, guilty, without appetite, suicidal, and so forth to add up a total depression score. One of the most widely used scoring methods is the Hamilton Depression Rating Scale or HDRS. Because depressed people usually recover spontaneously, given enough time, the depression ratings of patients who are given no active treatment usually drop over time. Thus, even when depressed people who volunteer for research studies are given an inactive placebo pill or placebo (inactive) light, their depression ratings decrease after eight to 16 weeks. In a clinical trial, volunteers are randomly given either the active treatment (such as bright light or an antidepressant drug) or the inactive placebo for contrast. To calculate how much of the average patient’s recovery was due to the active treatment, I considered the baseline depression rating (e.g., the HDRS score) as the 100% reference, and then the depression ratings at the end of the trial were computed for active treatment and for control treatment as a percentage of this baseline. Then, the net benefit of the active treatment was computed as the percentage reduction of depression ratings with active treatment minus the percentage reduction of depression with the control treatment.[36] Above, the figure of results of the Lam et al. study similarly display net benefit as a percentage reduction of MADRS score.
Our first studies of bright light tested only one single hour of bright light to treat hospitalized patients with nonseasonal depressions.[37] The patients were awakened to receive the light treatment from two hours to one hour before the patient’s usual planned time of awakening, so that these patients experienced one or two hours of wake therapy at the end of the night. We now call getting patients up early “wake therapy,” because to call this helpful treatment “sleep deprivation” gives the wrong impression. Most patients were drug free, but some were taking antidepressants during light treatment. As compared to a control hour of light placebo, which presumably produced the same sleep curtailment, the bright light reduced mood ratings about 12%. As will be explained, a 12% net gain as compared to placebo is similar to benefits achieved by antidepressant medications after weeks of treatment, so it was remarkable that such substantial benefit could be obtained with one single hour of bright light.
In an extension of our initial studies, 25 drug-free patients were treated with bright light each day for one week, compared to 26 patients treated with a dim-light placebo.[38] Depression ratings were 18% lower after bright light than after placebo, a benefit which was statistically significant. These and other data suggested that one-week treatment produced more benefit than only one hour of bright light. More recently, another one-week study of unmedicated inpatients observed a somewhat larger net advantage of 24.2%, which was likewise statistically significant.[39] Even a study reporting no statistically significant benefit achieved a 12.2% net advantage in HDRS ratings of the bright-light treated group[40], so that the failure to achieve statistical significance could have been partly due to an insufficient numbers of subjects. These studies of drug-free depressives were consistent in demonstrating advantages of bright light treatment.
Two European studies were important because they examined effects of bright light (as compared to a dim-light placebo) in patients who were also receiving antidepressant medications. In both of these studies, the net relative advantage of bright light over dim light was 27%. [41] Since the medication-only groups also did well in these combination studies, the additional improvement gained by the light-treated patients was especially impressive. A third European study also demonstrated substantial benefits of bright light compared with placebo among patients simultaneously receiving antidepressants.[42] Not only do these studies show that bright light improves the antidepressant response of patients who are receiving antidepressant medications, but they leave the impression that the benefit of bright light may be greater when patients are also receiving antidepressants.
A light triple treatment for nonseasonal depression was then tested.[43] Ironically, this new light treatment was developed by Dr. Neumeister working under Dr. Kasper at the University of Vienna – the same place where Sigmund Freud trained so many years ago. The Vienna psychiatrists treated patients in the hospital with serious nonseasonal depressions who were being treated with antidepressant drugs but had not yet responded. At the start, the doctors in Vienna awakened these patients in the middle of the first night and kept them awake for the rest of that night, while starting bright light treatment and also continuing with antidepressant drug treatment. About 70% of these patients felt dramatically better on the day after they had been awakened early, and they continued to feel better for the following days. About 35% of their depressive symptoms were relieved immediately. It had been previously known in Europe that such awakenings often relieved depression on the day of the early wakening, but the patients usually had relapsed almost completely the next day. Because of this relapse, few doctors in America thought that wake therapy was really very useful. If adding bright light can prevent the relapse, we have a new way to relieve the symptoms of severe depression in one day. There is nothing like it. This excellent response to bright light combined with wake therapy and antidepressants has now been reproduced by other studies at European hospitals.[44] Our group has also reproduced this effect in a small study of outpatients, who awakened themselves at 2 am in their own homes.[45]
Several studies have shown that bright light may be useful for depressed elderly in nursing homes.[46]
In addition to these studies, there has been one controlled study showing that 10,000 lux produced more benefit than 2,500 lux, when treatment was only 30 min. per day.[47] This study in effect confirms that bright light is an active treatment. Also, two studies have found shorter hospitalization times needed when depressed patients were in bright rooms than in rooms with darker windows.[48] A well-designed study showed that bright light was useful for premenstrual depression.[49]
There have been only three early studies with good scientific methodology which failed to confirm significant benefits of light for nonseasonal depression. Two of these studies indeed showed bright light was associated with benefit by every measure, but the statistical evidence was insufficient,[50] possibly because these studies needed more patients. The other was an unlucky study, in which, by chance, the patients who received bright light had a poorer prognosis at the outset than the patients with whom they were compared.[51]
A recent study of three-week light treatment of elderly outpatients was quite successful.[52] Dr. Klaus Martiny in Denmark has done an excellent five-week study showing that five weeks of light treatment was effective for nonseasonal depression.[53] Dr. Martiny has done an eight-week study combining light, wake therapy and antidepressant drugs which showed remarkable benefit.[54]
In summary, there is now extensive evidence that bright light treatment reduces symptoms for both nonseasonal and seasonal depression. For nonseasonal depression, the triple combination of bright light, half-night’s wake therapy, and medication might produce approximately a 35% reduction in symptoms in one week. There is a need for longer-term studies of the triple therapies. The good news is that with the new studies and new developments in light treatment, we may now be quite sure that we can improve the treatment of depression.
Additional
sources of information on light treatment
Society for Light Treatment
& Biological Rhythms, www.sltbr.org![]()
![]()
Center for Environmental Therapeutics, www.cet.org![]()
![]()
University of British Columbia Seasonal Affective Disorders Page, www.ubcsad.ca![]()
![]()
Endnotes for Chapter 4
29. Lam RW, Levitt AJ, Levitan RD, et al. Efficacy of Bright Light Treatment, Fluoxetine, and the Combination in Patients With Nonseasonal Major Depressive Disorder: A Randomized Clinical Trial. JAMA Psychiatry 2016;![]()
![]() 73(1):56-63. [return]
73(1):56-63. [return]
30. Meyerhoff J, Young MA, Rohan KJ. Patterns of depressive symptom remission during the treatment of seasonal affective disorder with cognitive-behavioral therapy or light therapy. Depress Anxiety 2018;![]()
![]() 35(5):457-67. [return]
35(5):457-67. [return]
31. Rohan KJ, Meyerhoff J, Ho SY, Evans M, Postolache TT, Vacek PM. Outcomes One and Two Winters Following Cognitive-Behavioral Therapy or Light Therapy for Seasonal Affective Disorder. Am J Psychiatry 2016;![]()
![]() 173(3):244-51. [return]
173(3):244-51. [return]
32. Fournier, J. C., DeRubeis, R. J., Hollon, S. D., Dimidjian, S., Amsterdam, J. D., Shelton, R. C., and Fawcett, J. Antidepressant drug effects and depression severity: a patient-level meta-analysis. Journal of the American Medical Association. 303(1)![]()
![]() . 47-53, 2010. [return]
. 47-53, 2010. [return]
33. Mulrow, CD et al. Treatment of Depression: Newer Pharmacotherapies.
USPHS AHCPR, Rockville, MD, 1999. Evidence
Report/Technology Assessment No. 7![]()
![]() . AHCPR Publication No. 99-E014:1-2-32. [return]
. AHCPR Publication No. 99-E014:1-2-32. [return]
34. Canadian Consensus Guidelines for the Treatment of Seasonal Affective
Disorder. Clinical and Academic Publishing, Vancouver, 1999. The full
text is available for purchase at Amazon.com![]()
![]() . A summary of the report in PDF form is available at the website for Austrian light manufacturer Instantdaylight
. A summary of the report in PDF form is available at the website for Austrian light manufacturer Instantdaylight![]()
![]() . [return]
. [return]
35. Depression Guideline Panel. Depression in Primary Care: Volume 2. Treatment of Major Depression. Clinical Practice Guideline Number 5, U.S. Dept. HHS, AHCPR Publication 93-0551, 1993. [return]
36. Kripke, DF. Light treatment for nonseasonal depression: speed, efficacy, and combined treatment. J.Affect.Dis. 1998;49:109-117. [return]
37. Kripke, DF. Photoperiodic mechanisms for depression and its treatment. In, Perris C, Struwe G, Jansson B (eds): Biological Psychiatry. Elsevier-North Holland Biomedical Press; 1981, 1249-1252; Kripke, DF et al. Bright white light alleviates depression. Psychiatry Res.1983;10:105-112. [return]
38. Kripke, DF et al. Controlled trial of bright light for nonseasonal major depressive disorders. Biol.Psychiatry. 1992;31:119-134. [return]
39. Yamada, N et al. Clinical and chronobiological effects of light therapy on nonseasonal affective disorders. Biol Psychiatry. 1995;37:866-873. [return]
40. Mackert, A et al. Phototherapy in nonseasonal depression. Biol.Psychiatry. 1991; 30:257-268. [return]
41. Prasko, J et al. Hastened onset of the effect of antidepressive drugs when using three types of timing of intensive white light. Cs.Psychiat.1988; 84(6):373-383.; Schuchardt, HM et al. Lichttherapie in der psychiatrischen praxis. Fortschritte der Neurologie Psychiatrie. 1992;60(S2):193-194; Kasper, S et al. The effects of light therapy in treatment indications other than seasonal affective disorder (SAD). In, Holick MF, Jung EG (eds): Biologic Effects of Light 1993. Berlin, Walter de Gruyter; 1994:206-218. [return]
42. Reide, M et al. Light Therapy in the Treatment of Nonseasonal Major Depressive Disorder. In, Holick MF, Jung EG (eds): Biologic Effects of Light 1993. Berlin, Walter de Gruyter & Co.; 1994. [return]
43. Neumeister, A et al. Bright light therapy stabilizes the antidepressant effect of partial sleep deprivation. Biol Psychiatry. 1996;39:16-21. [return]
44. Bloching, B et al. Outlasting antidepressant effect of late partial sleep deprivation by bright light therapy. J.Sleep Res. 2000;9:21; Colombo, C et al. Total sleep deprivation combined with lithium and light therapy in the treatment of bipolar depression: replication of main effects and interaction. Psychiatry Res. 2000;95:43-53. [return]
45. Loving RT, Kripke DF, Shuchter SR. Bright light augments antidepressant
effects of medication and wake therapy. Depress
Anxiety. 2002![]()
![]() ;16(1):1-3. [return]
;16(1):1-3. [return]
46. Moffit, MT. Bright light treatment of late-life depression.
Thesis, UMI Dissertation Services #9326258. Sumaya, IC et al. Bright light
treatment decreases depression in institutionalized older adults: a placebo-controlled
crossover study. J
Gerontol A Biol Sci Med Sci. 2001![]()
![]() Jun;56(6):M356-60. Royer, M., Ballentine, H., Eslinger, P. J., Houser,
K., Mistrick, R., Behr, R., and Rakos, K. Light Therapy for Seniors in Long-Term
Care. J
Am Med Dir Assoc. 2012 Feb;13(2):100-2. Van der Lek RF, Swaab DF, Twisk J, Hol, EM, Hoogendijk,
W J, and van Someren, EJ. Effect of bright light and melatonin on cognitive and
noncognitive function in elderly residents of group care facilities: a randomized
controlled trial.
JAMA. 2008
Jun;56(6):M356-60. Royer, M., Ballentine, H., Eslinger, P. J., Houser,
K., Mistrick, R., Behr, R., and Rakos, K. Light Therapy for Seniors in Long-Term
Care. J
Am Med Dir Assoc. 2012 Feb;13(2):100-2. Van der Lek RF, Swaab DF, Twisk J, Hol, EM, Hoogendijk,
W J, and van Someren, EJ. Effect of bright light and melatonin on cognitive and
noncognitive function in elderly residents of group care facilities: a randomized
controlled trial.
JAMA. 2008![]()
![]() ;299(22):2642-2655. [return]
;299(22):2642-2655. [return]
47. Beauchemin, KM et al. Phototherapy is a useful adjunct in the treatment of depressed in-patients. Acta Psychiatr Scand. 1997;95:424-427. [return]
48. Beauchemin, KM et al. Sunny hospital rooms expedite recovery from severe and refractory depressions. J.Affect.Disord. 1996;40:49-51; Benedetti, F et al. Morning sunlight reduces length of hospitalization in bipolar depression. J.Affect.Disord. 2001;62:221-223. [return]
49. Lam, RW, Carter D, Misri S, Kuan AJ, Yatham LN, Zis AP. A controlled study of light therapy in women with late luteal phase dysphoric disorder. Psychiatry Res. 1999;86:185-192. [return]
50. Mackert, A et al. Phototherapy in nonseasonal depression. Biol.Psychiatry. 1991;30:257-268.; Fritzsche, M et al. Sleep deprivation as a predictor of response to light therapy in major depression. J.Affect.Disord. 2001;62:207-215. [return]
51. Holsboer-Trachsler, E et al. Sleep deprivation and bright light as potential augmenters of antidepressant drug treatment - neurobiological and psychometric assessment of course. J Psychiat Res. 1994;28:381-399. [return]
52. Lieverse R, van Someren E J, Nielen, MM, Uitdehaag, BM, Smit, JH,
and Hoogendijk, WJ. Bright light treatment in elderly patients with nonseasonal
major depressive disorder: a randomized placebo-controlled trial. Arch Gen.Psychiatry 68(1)![]()
![]() , 61-70. 2011. [return]
, 61-70. 2011. [return]
53. Martiny K, Lunde M, Unden M, Dam, H, and Bech, P. Adjunctive bright light in non-seasonal major depression: results from patient-reported symptom and well-being scales. Acta Psychiatr Scand. 2005 Jun;111(6):453-9; Martiny K, Lunde M, Unden M, Dam H, and Bech, P. Adjunctive bright light in non-seasonal major depression: results from clinician-rated depression scales. Acta Psychiatr Scand. 2005 Aug;112(2):117-25. [return]
54. Martiny, K., Refsgaard, E., Lund, V., Lunde, M., Sorensen, L., Thougaard, B., Lindberg, L., and Bech, P. A 9-week randomized trial comparing a chronotherapeutic intervention (wake and light therapy) to exercise in major depressive disorder patients treated with duloxetine. Journal of Clinical Psychiatry 73(9), 1234-1242. 2012. [return]
Table of Contents
Brighten Your Life, in all its formats, including this ebook, copyright ©1997-2019 by Daniel F. Kripke, M.D. All rights reserved.